Rethinking Hematocrit in Testosterone Therapy: Dr. Abraham Morgentaler's Bold Perspective
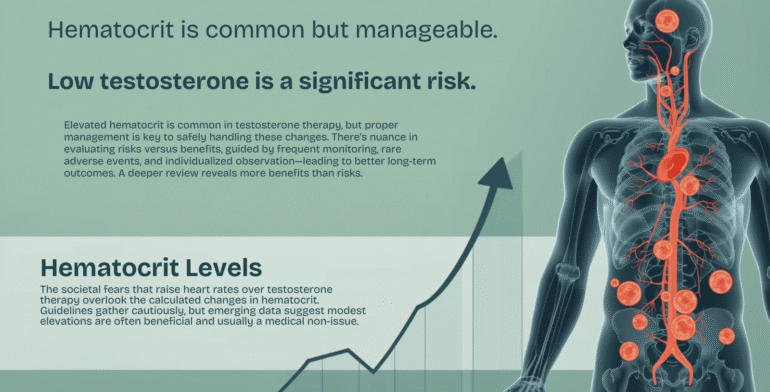
In the world of men's hormone optimization, few topics spark as much debate as hematocrit levels during testosterone therapy (TTh). For decades, medical guidelines have treated elevated hematocrit—a measure of the percentage of red blood cells in your bloodstream—as a red flag, potentially signaling increased risks like blood clots or cardiovascular events. But what if those guidelines are overly cautious? What if a modest rise in hematocrit isn't just harmless, but actually beneficial for longevity and vitality?
Enter Dr. Abraham Morgentaler, a Harvard urologist and pioneering voice in testosterone research. With over 30 years of clinical experience and hundreds of peer-reviewed publications, Morgentaler challenges the conventional wisdom. He argues that the standard thresholds for intervening in TTh—such as stopping treatment when hematocrit exceeds 54%—are outdated and fear-driven, ignoring emerging evidence that higher hematocrit levels (up to 52-54% or beyond) correlate with reduced mortality, not heightened danger. At Increase My T, we align with this forward-thinking approach, prioritizing symptom relief and overall well-being over rigid numbers. In this in-depth exploration, we'll unpack Morgentaler's perspective, review the science, and empower you to navigate TTh with confidence.
Understanding Hematocrit: The Basics and Why Testosterone Matters
Hematocrit (HCT) is a simple blood test metric representing the volume of red blood cells (erythrocytes) in your total blood volume. In a healthy adult male, normal ranges typically fall between 40-50%, comprising about 45% erythrocytes, 54% plasma (the liquid portion), and 1% white blood cells and platelets. Think of it as the "oxygen-carrying capacity" of your blood—red cells bind oxygen in the lungs and deliver it to tissues throughout the body.
Testosterone naturally stimulates erythropoiesis, the production of red blood cells in the bone marrow. This is why TTh often leads to a predictable 3-6% increase in hematocrit within the first few months of treatment, stabilizing thereafter. For many men, this boost translates to tangible benefits: enhanced energy, better exercise tolerance, and improved cognitive sharpness. Yet, this physiological response has long been pathologized as "secondary polycythemia" or erythrocytosis—a potential side effect warranting intervention.
Morgentaler reframes this: Erythrocytosis isn't a bug; it's a feature. Low testosterone (hypogonadism) is often linked to anemia and fatigue, and TTh corrects this by normalizing red cell production. In fact, recent trials like the Testosterone Trials have shown TTh resolving unexplained anemia in older men, with hemoglobin rises associated with better physical function and mood—without spiking adverse events.
Current Guidelines: Playing It Safe or Missing the Mark?
Major organizations like the Endocrine Society and American Urological Association (AUA) set the tone for TTh monitoring. Their recommendations are clear: Measure baseline hematocrit before starting therapy. Recheck at 3-6 months, then annually. If HCT climbs above 54%, halt treatment until it drops, evaluate for underlying issues like sleep apnea or hypoxia, and restart at a lower dose. For men starting with HCT >50%, TTh is often contraindicated altogether.
These thresholds stem from early concerns in the 1990s and 2000s, when supraphysiological testosterone doses (common in bodybuilding circles) were linked to rare clotting events. Meta-analyses from that era noted TTh users were nearly four times more likely to hit HCT >50% than placebo groups, prompting a conservative stance to err on the side of caution. The logic? Thicker blood could theoretically increase viscosity, straining the heart and raising thrombosis risk.
But Morgentaler calls this "guideline creep"—recommendations hardened into dogma without robust, long-term data. In a pointed critique of the AUA's 2018 guidelines, he and co-authors argue that the 54% cutoff lacks evidence tying it to real-world harm in properly dosed TTh. Why 54%? It's arbitrary, they say, ignoring individual factors like hydration, altitude, or even the time of day (dehydration from a morning coffee can skew readings by 2-3%).
Dr. Morgentaler's Challenge: Higher Isn't Always Riskier
Morgentaler's contrarian stance isn't mere opinion; it's rooted in decades of clinical observation and evolving research. He posits that current guidelines are "likely too conservative," with benefits extending to HCT in the low 50s—or higher—due to enhanced oxygen delivery. Low oxygen transport, common in hypogonadal men, contributes to fatigue, muscle loss, and even cognitive fog. By bumping HCT, TTh may counteract these, fostering resilience against age-related decline.
At the heart of his argument: Focus on symptoms, not silos. Does the man feel energized? Is he hitting the gym without crashing? Overall well-being trumps a lab value. Morgentaler advocates practical tweaks like therapeutic phlebotomy (blood donation) or switching to oral TTh formulations, which raise HCT less than injectables, rather than blanket discontinuation. This patient-centered ethos echoes his broader mission: Testosterone deficiency isn't just about libido—it's a systemic thief of vitality, reclaimable through informed therapy.
Blood Viscosity and Oxygen Delivery: Balancing the Equation in Hematocrit in Testosterone Therapy
A core concern with elevated hematocrit in testosterone therapy is the potential for increased blood viscosity, which could theoretically impair blood flow and heighten cardiovascular strain. However, the relationship between HCT and blood viscosity is not linear but exponential—meaning that at moderate elevations typical in TTh (up to 52-54%), the rise in viscosity is relatively minor and often clinically insignificant. Sharp increases in viscosity typically occur only at much higher HCT levels, well beyond therapeutic ranges.
Moreover, this modest viscosity change is frequently outweighed by the substantial benefits of improved oxygen delivery. Higher HCT enhances the blood's oxygen-carrying capacity, supporting better tissue perfusion, energy metabolism, and overall vitality—factors that may contribute to reduced mortality in hypogonadal men on TTh. Research indicates that these oxygenation advantages can mitigate or even reverse potential rheological drawbacks, shifting the paradigm from viewing HCT rises as risks to recognizing them as adaptive responses.
The Evidence Mounts: Hematocrit as a Mortality Protector?
Recent studies bolster Morgentaler's optimism. A landmark 2021 analysis of 737 hypogonadal men followed for up to 8 years found that those on TTh saw HCT rise to an average 49% (range 47-51%), with no cases exceeding 52%. Strikingly, men who died had lower HCT than survivors (p=0.021), and greater HCT increases correlated with reduced all-cause mortality—even after adjusting for age and diabetes. Those hitting 50-52% fared better than those stuck at 46-49%. A 2025 follow-up echoed this: Long-term TTh slashed mortality risk, with HCT elevations (up to 52%) independently protective, possibly via extended red cell lifespan or anti-inflammatory effects.
The TRAVERSE trial (2023, with 2024 analyses) adds nuance: Among 5,246 older men, TTh raised HCT >54% in just 13 cases (vs. none in placebo), with no uptick in major adverse cardiovascular events (MACE) or venous thromboembolism (VTE). Time-dependent models showed no link between HCT changes and MACE/VTE risk. Even a 2025 real-world cohort flagging a 55% MACE hike with long-term TTh couldn't tie it to HCT, attributing risks to unmeasured confounders like dosing or comorbidities.
These findings flip the script: What was once a "risk factor" now looks like a biomarker of therapeutic success. As Morgentaler notes, TTh's vasodilatory and anti-atherosclerotic perks likely offset any viscosity concerns.
| Study | Key Finding | HCT Threshold | Mortality/CV Impact |
|---|---|---|---|
| Strange et al. (2021) | Greater HCT rise → lower mortality | Up to 52% | Reduced all-cause death (HR inverse) |
| TRAVERSE (2023/2024) | No MACE/VTE link to HCT changes | >54% rare | Neutral CV safety |
| Hackett et al. (2025) | TTh cuts mortality in T2DM men | Low 50s beneficial | 39% risk reduction |
| Louvaras et al. (2025) | Long-term TTh ↑ MACE, but not HCT-driven | N/A | 55% HR, confounders noted |
Managing Elevated Hematocrit: Practical Strategies for Real Life
So, how do we harness these insights without courting risks? Morgentaler emphasizes proactive, individualized care:
- Monitor Smartly: Baseline and 3-month checks are non-negotiable, but confirm highs with a retest (hydrate first!). Aim to keep HCT <54% via dose tweaks, not panic stops.
- Lifestyle Levers: Hydration, exercise, and avoiding smoking blunt spikes. For persistent elevations, donate blood—it's effective, free, and boosts community health.
- Formulation Flexibility: Gels or orals may suit HCT-sensitive men better than injectables.
- Symptom Surveillance: Track energy, mood, and performance. If you're thriving at 51% HCT, why intervene?
At Increase My T, our protocols blend these tactics with unlimited coaching, ensuring your therapy evolves with you.
Debunking Cardiovascular Fears: The Data Speaks
Clotting worries persist, but evidence demurs. Meta-analyses show TTh halves CV mortality in deficient men, with no erythrocytosis-driven uptick in events. The 2024 AUA update concedes: Definitive CV risk direction remains unclear, urging shared decision-making. Morgentaler's take? Fear of the unknown has stalled progress; real risks are low T's toll—increased fat, diabetes, and heart strain.
Conclusion: Reclaim Your Vitality with Informed TTh
Dr. Morgentaler's perspective isn't about recklessness—it's about reclaiming balance. Elevated hematocrit on TTh isn't a villain; it may be your ally in fighting fatigue and extending healthspan. As 2025 research reinforces, benefits often outweigh bogeyman risks, especially when managed holistically.
At Increase My T, we're committed to this evidence-based evolution. Whether you're exploring our Tirzepatide + Oxytocin special for metabolic synergy or foundational TTh, our team delivers personalized protocols, cold-chain shipped meds, and lifelong support. Ready to optimize? Complete our New Patient Intake Form today and let's elevate you.
Intake FormsDisclaimer: This article is for informational purposes only. Consult a healthcare provider before starting any therapy. Individual results vary.
References
(Inline citations link to primary sources; full bibliography available upon request.)